|
PS20 - Association of socioeconomic factors and academic performance on medical students entering primary care specialties
Poster Presenter:
Shilpa Kolachina, Loyola University Chicago Stritch School of Medicine, Medical Student, Hanover Park, IL
[email protected]
Additional Poster Presenters:
Elizabeth Miller, Medical Student, Loyola University Chicago Stritch School of Medicine
[email protected]
Objectives:
In this study, we specifically aim to Identify any statistically significant associations of sociodemographic factors and academic performance on students entering primary care specialties, specifically utilizing the Loyola University Chicago Stritch School of Medicine (LUC-SSOM) institutional data from medical students that graduated between 2013-2019. We hope to determine the latter through the following goals:
• Identify associations between sociodemographic factors including age, gender, race, marital status, number of children, family income, and disadvantaged/economically disadvantaged status on medical school application on entering primary care specialties.
• Identify associations between academic performance on LUC- SSOM pre- clinical coursework final numerical grades and entering primary care specialties.
• Demonstrate any associations between overall LUC-SSOM clerkship scores and entering primary care specialties
• Determine whether certain specialties are associated with a higher USMLE Step 1 score(s) or a difference in failure rate of USMLE Step 1, especially considering the new pass or fail change in scoring methodology
Methods:
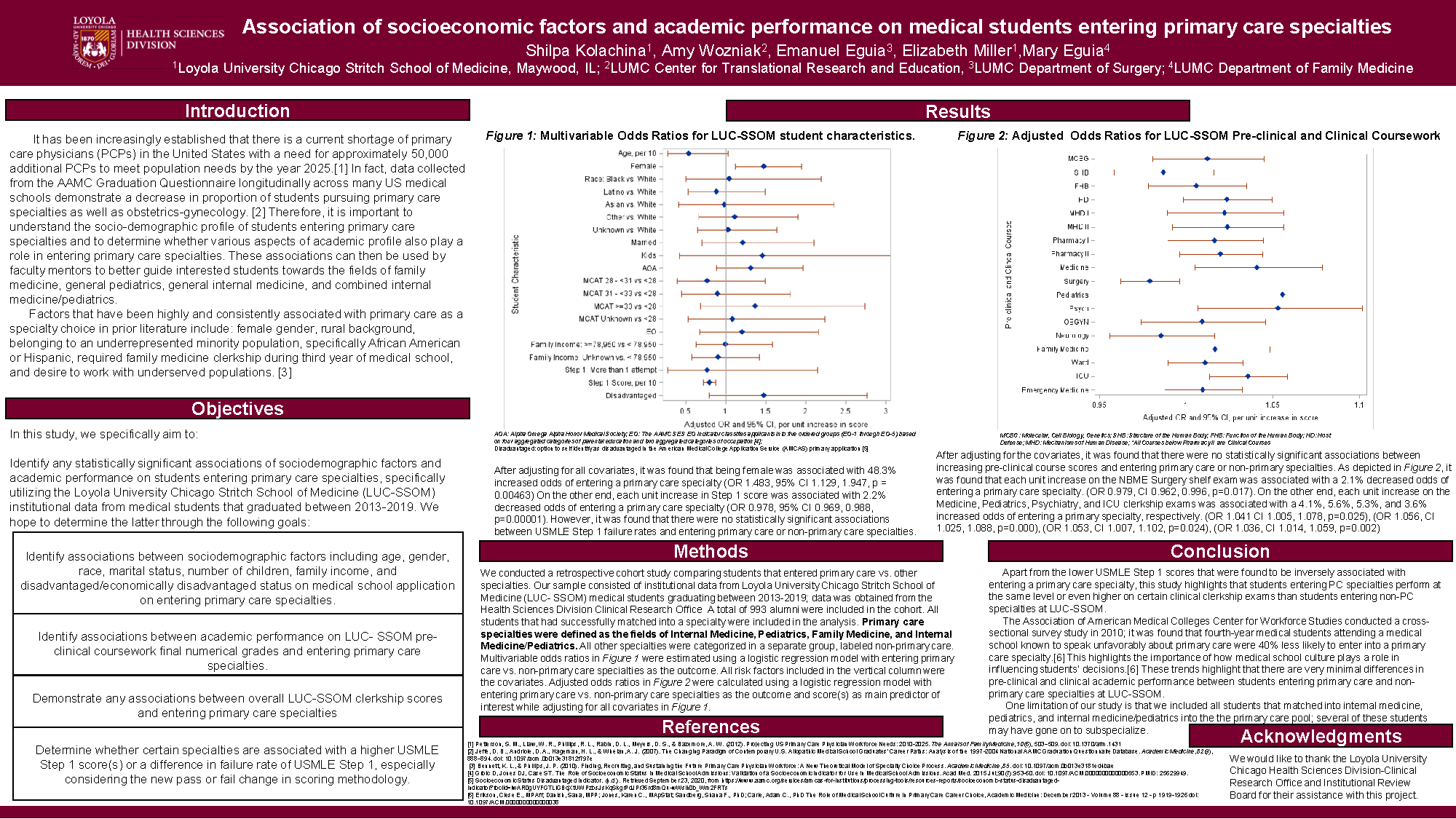
We conducted a retrospective cohort study comparing students that entered primary care vs. other specialties. Our sample consisted of institutional data from Loyola University Chicago Stritch School of Medicine (LUC- SSOM) medical students graduating between 2013-2019; data was obtained from the Health Sciences Division Clinical Research Office A total of 993 alumni were included in the cohort. All students that had successfully matched into a specialty were included in the analysis. Primary care specialties were defined as the fields of Internal Medicine, Pediatrics, Family Medicine, and Internal Medicine/Pediatrics. All other specialties were categorized in a separate group, labeled non-primary care. Multivariable odds ratios in Figure 1 were estimated using a logistic regression model with entering primary care vs. non-primary care specialties as the outcome. All risk factors included in the vertical column were the covariates. Adjusted odds ratios in Figure 2 were calculated using a logistic regression model with entering primary care vs. non-primary care specialties as the outcome and score(s) as main predictor of interest while adjusting for several covariates.
Results:
After adjusting for all covariates, it was found that being female was associated with 48.3% increased odds of entering a primary care specialty (OR 1.483, 95% CI 1.129, 1.947, p = 0.00463) On the other end, each unit increase in Step 1 score was associated with 2.2% decreased odds of entering a primary care specialty (OR 0.978, 95% CI 0.969, 0.988, p=0.00001). However, it was found that there were no statistically significant associations between USMLE Step 1 failure rates and entering primary care or non-primary care specialties.
After adjusting for several covariates, it was found that there were no statistically significant associations between increasing pre-clinical course scores and entering primary care or non-primary specialties. As depicted in Figure 2, it was found that each unit increase on the NBME Surgery shelf exam was associated with a 2.1% decreased odds of entering a primary care specialty. (OR 0.979, CI 0.962, 0.996, p=0.017). On the other end, each unit increase on the Medicine, Pediatrics, Psychiatry, and ICU clerkship exams was associated with a 4.1%, 5.6%, 5.3%, and 3.6% increased odds of entering a primary care specialty, respectively. (OR 1.041 CI 1.005, 1.078, p=0.025), (OR 1.056, CI 1.025, 1.088, p=0.000), (OR 1.053, CI 1.007, 1.102, p=0.024), (OR 1.036, CI 1.014, 1.059, p=0.002)
Conclusions:
Apart from the lower USMLE Step 1 scores that were found to be inversely associated with entering a primary care specialty, this study highlights that students entering PC specialties perform at the same level or even higher on certain clinical clerkship exams than students entering non-PC specialties at LUC-SSOM. In addition, since it was found that there were no statistically significant associations between USMLE Step 1 failure rates and entering primary care or non-primary care specialties, the results found regarding Step 1 scores are less relevant considering the new change in USMLE scoring to pass/fail.
The Association of American Medical Colleges Center for Workforce Studies conducted a cross- sectional survey study in 2010; it was found that fourth-year medical students attending a medical school known to speak unfavorably about primary care were 40% less likely to enter into a primary care specialty.[1] This highlights the importance of how medical school culture plays a role in influencing students’ decisions.[1] These trends highlight that there are very minimal differences in pre-clinical and clinical academic performance between students entering primary care and non- primary care specialties at LUC-SSOM.
One limitation of our study is that we included all students that matched into internal medicine, pediatrics, and internal medicine/pediatrics into the the primary care pool; several of these students may have gone on to subspecialize.
References:
[1]Erikson, Clese E., MPAff; Danish, Sana, MPP; Jones, Karen C., MApStat; Sandberg, Shana F., PhD; Carle, Adam C., PhD The Role of Medical School Culture in Primary Care Career Choice, Academic Medicine: December 2013 - Volume 88 - Issue 12 - p 1919-1926 doi: 10.1097/ACM.0000000000000038
|